Abstract
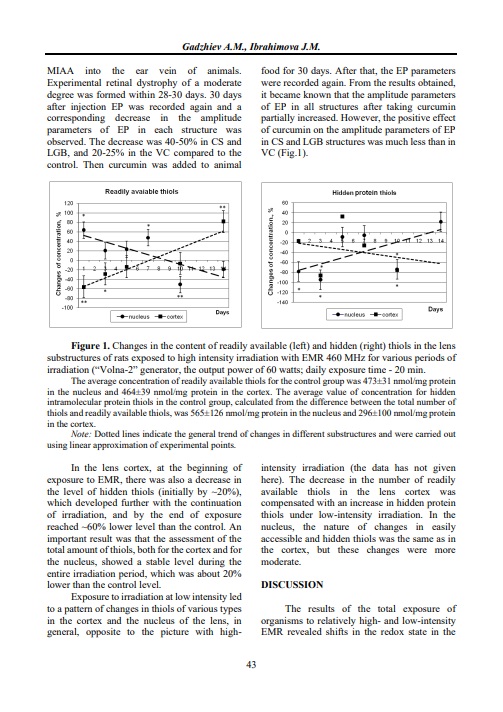
Electromagnetic radiation (EMR) in the microwave range, even at non-thermal intensity, causes significant biochemical and physiological changes in living organisms, which are supposed to be associated with its possible oxidative effect. This work is devoted to the study of the mechanism of realization of the EMR effect in the eye lens at the level of redox state elements, based on the fact that this organ is the most suitable model: it functions semi-autonomously and has a well-organized system of antioxidant protection. The transparency of the lens is maintained by preserving the redox balance, in which the homeostasis of thiol compounds of protein and non-protein nature plays an important role. Our experiments were performed on rats using 460 MHz EMR for exposure at non-thermal intensities (power flux density between 10 and 30 µW/cm2). It has been shown that chronic exposure to EMR for up to two weeks caused changes in the redox state of the lens, which manifested in changes in the level of lipid peroxidation processes and the content of thiols of various natures. The substructures of the lens (cortical and nuclear regions) reacted to EMR exposure in different ways. Depending on the EMR intensity, pro- and antioxidant characters were revealed in their reactions. The dynamics of the oxidative reaction of lens substructures were also different under high- and low-intensity exposure. The character of the kinetics of changes in the products of oxidative reactions (malondialdehyde and lipid hydroperoxides) and reducing agents (non-protein and protein SH groups) in the lens of the irradiated organism suggested the role of the enzymatic thiolation-dethiolation system to preserve the redox balance in the substructures of the lens. In addition, the results on changes (kinetics) in the content of various protein SH-groups, i.e., hidden inside the protein molecule and exposed on its surface, during EMR exposure, as well as the data available in the literature, allow us to put forward suggestions about the supramolecular mechanism of homeostasis regulation, in particular, thiol homeostasis regulation in such high-protein structures as the lens, which can be realized by aggregation-disaggregation of protein molecules (crystallins in the case of the lens). Our results can serve as a basis for developing a new non-invasive approach to cataract prevention using low-intensity microwave radiation.
References
Avetisov SE., Sheremet NL., Muranov KO., Polianskiy NB., Bannik KI., Kurova VS., Polunin GS., Ostrovskiy MA. [Experimental study of the influence of disturbing factors and chaperone-like drugs on cataractogenesis] Vestn. Oftalmol. 2013; 129(5):155-159.
Gadzhiev AM. [Thiol homeostasis in the eye lens and redox effects of microwave irradiation]. Materials of the 5th Congress of Azerbaijan Physiologists dedicated to the 50th Anniversary of the A.I.Karayev Institute of Physiology. Baku, 2017; 175-176.
Ibragimova JM., Gadjiev AM., Ibragimov AS. Changes in lipid peroxidation under exposure to electromagnetic radiation of non-thermal intensity in the prenatal period. Biophysics. 2021; 66(2):352-355. https://doi.org/10.1134/S0006350921020081
Musaev AV., Ibragimova JM., Gadzhiev AM. Modification of experimental oxidative stress in lens tissues by 460 MHz EMR irradiation. Physiotherapy, balneology, rehabilitation. Moscow. 2009; 2:10-13.
Rodchenko D., Kirichenko M., Sarchuk E. [The effect of microwave radiation on the human body: aspects of the problem. Scientific review]. Fundamental and applied research. 2020; No.3.
Abbasova MT., Gadzhiev AM. The effects of electromagnetic radiation on lipid peroxidation and antioxidant status in rat blood. Biophysics. 2022; 67(1):100-105. period. Biophysics. 2021; 66(2):352-355. https://doi.org/10.1134/S000635092201002X
Allen EM., Mieyal JJ. Protein-thiol oxidation and cell death: Regulatory role of glutaredoxins. Antioxid. Redox. Signal. 2012; 17: 1748-63.
Clanton T., Zuo L., Klawitter P.: Oxidants and Skeletal Muscle Function: Physiologic and Pathophysiologic Implications. PSEBM. 1999; 222:253-262.
Gadzhiev AM. Oxidative Effects of Chronic Whole Body Exposure to Decimeter Electromagnetic Radiation on Separate Brain Structures. Turkish Journal of Neurology, 2010, v.16, Suppl.1, p.230. 9th National Neuroscience Congress, April 13-17, 2010, University of Yeditepe, Istanbul, Turkey
Gadzhiev AM. [Thiol homeostasis in the eye lens and the oxidative effect of exposure to decimeter electromagnetic radiation]. Azerbaijan Journal of Physiology. 2013; 31:229-40
Lou MF. Thiol regulation in the lens. J. Ocular Pharmacol.Therapeutics. 2000; 16:137-148. https://doi.org/10.1089/jop.2000.16.137
Lou MF. Redox regulation in the lens. Retinal and Eye Research. 2003; 22(5):657-682. https://doi.org/10.1016/s1350-9462(03)00050-8
Lou, M.F. Glutathione and Glutaredoxin in Redox Regulation and Cell Signaling of the Lens. Antioxidants 2022, 11, 1973. https://doi.org/10.3390/antiox11101973
Ogata FT., Branco V., Vale FF., Coppo L. Glutaredoxin: Discovery, redox defense and much more. Redox Biol. 2021; 43:10197. https://doi.org/10.1016/j.redox.2021.101975
Sedlak J., Lindsay RH. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Analytical Biochemistry.1968; 25(C):192–205
Shahbazi-Gahrouei D., Setayandeh SS., Aminolroayaei F., Shahbazi-Gahrouei S. Biological Effects of Non-ionizing Electromagnetic Fields on Human Body and Biological System: A Systematic Literature Review. Journal of Medical Sciences. 2018; 18:149-156. https://doi.org/10.3923/jms.2018.149.156
Wei M., Xing KY., Fan YC., Libondi T., Lou MF. Loss of thiol repair systems in human cataractous lenses. Investig. Ophthalmol. Vis. Sci. 2015; 56:598–605. https://doi.org/10.1167/iovs.14-15452
Xing K-Y., Lou MF. Effect of Age on the Thioltransferase (Glutaredoxin) and Thioredoxin Systems in the Human Lens. Invest. Ophthalmol. Vis. Sci. 2010; 51:6598–6604. https://doi.org/10.1167/iovs.10-5672
Yakymenko I., Tsybulin O., Sidorik E., Henshel D., Kyrylenko O., Kyrylenko S. Oxidative mechanisms of biological activity of low-intensity radiofrequency radiation. Electromagnetic Biology and Medicine. 2016; 35(2):186-202. https://doi.org/10.3109/15368378.2015.1043557
Yurekli, F., Ozkan, M., Kalkan, T. et al.: GSM base station electromagnetic radiation and oxidative stress in rats. Electromagnetic Biology and Medicine. 2006; 25(3):177-188. https://doi.org/10.1080/15368370600875042
Zhang J., Yan H., Lou MF. Does oxidative stress play any role in diabetic cataract formation? Re-evaluation using a thioltransferase gene knockout mouse model. Exp Eye Res. 2017; 161:36-42. https://doi.org/10.1016/j.exer.2017.05.014

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright (c) 2023 Azerbaijan Journal of Physiology